Enhancing Rural Healthcare Access through Telemedicine: The Impact of the Telemedicine Centre Initiative in India
The primary healthcare system in India challenges many obstacles, especially in rural and urban areas. Socioeconomic disparities, inadequate infrastructure, and geographic isolation make these problems worse. The Telemedicine Centre initiative was created in response to the COVID-19 epidemic, which has made these issues worse. Its goal is to use telemedicine technology to increase access to healthcare in underserved and rural areas. The project seeks to address the various issues that rural communities confront, such as a lack of qualified healthcare workers, high out-of-pocket costs, gaps in Non-communicable disease (NCD) control, and inadequate health infrastructure.
Problem statement
There are important gaps in the Indian health system that requires immediate attention, and these include accessibility of primary healthcare services, availability of a full range of services, clinical quality of care and cost of care.
The following are the main constraints in the healthcare system:
- Inadequate Health Infrastructure facilities (shortage of PHCs & CHCs)
- Shortage of skilled health personnel including doctors & specialists
- Lack of access to public health services for Women’s health, Child health, water, hygiene, sanitation and nutrition
- Incurring of relatively large out-of-pocket expenses for accessing healthcare
- Gaps in prevention and control of communicable and non-communicable diseases, including locally endemic diseases
- Limited access to integrated comprehensive primary healthcare
- Lack of promotion of healthy lifestyles
Problem statement
Piramal Swasthya offered technology-enabled comprehensive models to bring a meaningful impact in the intervention areas for a project duration of 3 years.
Our models were designed to understand the healthcare challenges/constraints faced by the general populace of all age groups (especially women) residing in rural/urban areas focusing on RMNCH+A (Reproductive, Maternal, Newborn, Child Health + Adolescent) & NCD (Non-communicable diseases)
Telemedicine is a revolutionary Information and Communications Technology (ICT)-driven service to overcome geographical/distance/physician shortage barriers and increase access to primary and specialist healthcare services. Telemedicine is incredibly beneficial for rural and underserved communities that traditionally suffer from a lack of access to vital primary and specialist healthcare services.
Telemedicine services at PHCs
Introduction
It is a combination of PHC services and telemedicine technology-platform where the primary health care services for episodic illness, important communicable and non-communicable diseases will be provided by PHC, and telemedicine (Specialist) consultation will be provided by PSMRI (Piramal Swasthya Management and Research Institute).
Objectives
- The primary objective of these telemedicine centers is to deliver preventive and primary healthcare solutions for long term relief for patients.
- Early diagnosis and better treatment management.
- Contributing to the overall reduction of Maternal Mortality Ratio (MMR), Under 5 Mortality Rate (including IMR & NMR), and reduction of NCD burden in the areas of operations by providing specialist consultations and timely referrals.
Target beneficiaries
- Persons suffering from communicable & non-communicable chronic disease
- Antenatal & Postnatal women
- Children under 5 yrs. of age (excluding neonates and infants)
Project Framework
The Telemedicine project, initiated by the Bayer Foundation in partnership with Piramal Swasthya, encompasses a comprehensive framework designed to address the health-care delivery challenges in the rural districts across four states of Northern and Eastern India.
Deployment Phase
The initial phase of the project focused on establishing the necessary infrastructure for telemedicine services at selected Primary Health Centers (PHCs). This involved:
Infrastructure Setup: Identification and setup of telemedicine nodes within PHCs, equipped with necessary IT and medical equipment, including computers with video conferencing capabilities, blood pressure monitors, glucometers, and other diagnostic tools.
Software Customisation and Deployment: Customisation of the “AMRIT (Accessible Medical Record via Integrated Technology) ” telemedicine application software to meet the project’s specific needs, including offline-online data synchronisation, integration with medical devices, and real-time dashboard functionality for monitoring and evaluation
Staff Recruitment and Training: Recruitment of telemedicine technologists and medical specialists followed by comprehensive training covering telemedicine protocols, use of diagnostic equipment, and software applications for data entry and management
Assessment of the Project Impact
Descriptive Analysis: Statistical analysis of beneficiary demographics, types of health conditions diagnosed, and treatments prescribed to ascertain the scope and reach of telemedicine services.
Outcome Analysis: Evaluation of health outcomes based on the characteristics of the patients who sought teleconsultation. We also analysed follow-up consultation data, measuring improvements in health conditions, adherence to treatments, and reductions in disease prevalence within the beneficiary population
Result
An analysis of over 100,000 telemedicine consultations by using AMRIT in the healthcare centres highlights the initiative’s significant impact, particularly in overcoming rural healthcare challenges. The findings align with previous studies, confirming telemedicine’s role in enhancing access to care. This success prompts a reassessment of traditional healthcare models, suggesting telemedicine could improve efficiency and expand primary care, especially in India, where healthcare infrastructure is uneven and often stretched. The project exemplifies how health technology can democratize healthcare access. Looking ahead, it’s crucial to build on these successes and refine strategies to further improve public health and ensure sustainable, equitable care delivery.
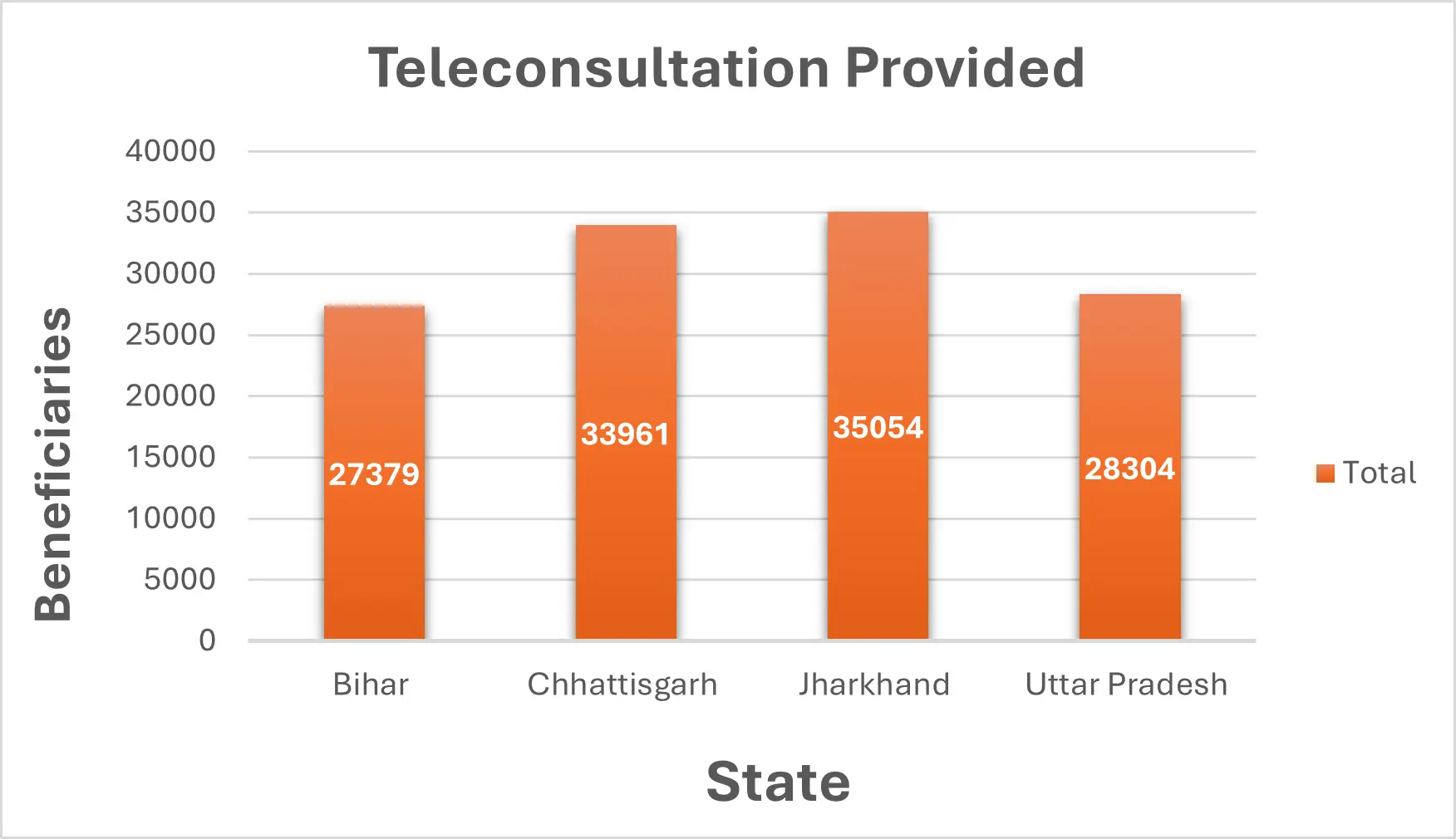
The TMC (Telemedicine Centers) model was implemented across four states to bolster community level quality health care facilities that catered to 100,678 unique rural beneficiaries) with 27,379 (22.0%) patients provided services in Bihar, 33,961 in Chhattisgarh (27.2%), 35,054 in Jharkhand (28.1%), and 28,304 in Uttar Pradesh (22.7%).
Among the districts catered to under the project, Katihar (50.4%) in Bihar, Kondagaon (50.4%) in Chhattisgarh, and Dumka (47.9%) in Jharkhand noted the most footfalls while in Uttar Pradesh, the project was implemented largely in Bahraich (99.9%).
The demographic, behavioural and clinical characteristics of the participants captured from the data collected during the consultations. The mean age of the total patients across all the states was 30.09 years, with a substantial proportion (25.1%) of the beneficiaries being in the age range of 20-29 years of age, which was also reflected across the states of Bihar (30.4%), Chhattisgarh (25.9%), and Uttar Pradesh (19.1%) while in Jharkhand (28%), majority of the beneficiaries belonged to 40-59 years of age potentially indicative of a prevalence of ailments in ageing population. Female patients made up the majority of visitors at the centres across all states, with 64.2% of the total visitors being women, possibly owing to the absence of working males from the household during the facility’s opening hours. Most of the patients were also first-time visitors (91.2%) coming in for largely single consultations (86.8%), indicative of the minor ailments requiring primary-level interventions.